A couple weeks ago, I wrote about how I was thinking about joining the low carb club. While I logically, critically understood that low carb was going to be better for my blood sugars (because when you have a hard time processing glucose, hello), there was part of me who really, really, really did not want to admit that maybe this was a good idea. The better idea. The only idea?
But the thing with people who are low carb is that it’s kind of like Christians (and I can say this because I am a Christian, so I know). When you meet someone who is in one of these two groups, they really, really, really think they’re right. Like, super right. Only right. Going-to-hell-fire-and-brimstone right. And it’s such a huge turnoff and I want to be like, “Oh yeah? WATCH ME.”
It’s this attitude that has permeated the low-carb-high-fat, ketotic and Bernstein groups that really just annoys the living shit out of me. It’s just smug and arrogant and the worst part is they’re kind of right. But they’re so annoying about it!
I joined several groups after my post because I wanted to “observe the other side” and see what was really going on. Some of their comments about people who eat “high carb” were so nasty. As you can imagine, I didn’t last very long in those groups. All of this happened well before I read Renza’s blog post about feeling welcome in the DOC. There was a distinct lack of welcoming other’s viewpoints and lifestyles in this group. A complete disregard for whether or not someone could live a healthy life even if it was not what you chose to do or what worked for you.
So it made me think about the whole high carb / low carb debate, and it also made me reflect on A1C goals in general. Where do those come from? Yes, we have the ADA / AACE recommendation for under 7%, but if you listened for 5 seconds to anyone in the Bernstein groups, you’d think ADA was trying to kill us all. Which I don’t think is true. But it was interesting hearing that they believe what Bernstein said about “diabetics deserving to have normal blood sugars.” Which I understand is very appealing, but then a friend of mine pointed out that her sanity was also important, and I get that too!
I’ve been thinking for awhile now about why it has taken more than two decades to finally care so much about having my A1C in the sixes. Mostly I think I thought it was too hard, that I wanted to live normal, and that living normal and having normal blood sugars at the same time was just not something you could do. I grew up — or at least since I got an insulin pump 15 years ago — hearing and believing that I deserved to eat what I wanted to eat, as long as I took insulin for it, and I kept expecting that this would work. I really believed that because I had an insulin pump, everything was fine and that I didn’t need to be different. And maybe this is true, but I have recently realized that is so goddamn hard that it might not actually be worth it anymore.
Let me show you a couple of Dexcom graphs, to illustrate my point.
After my birthday weekend, I cracked down on my carbohydrate intake. In addition, I also watched my blood sugar levels like a hawk, taking many small doses throughout the day. My breakfasts consisted of three eggs and sausage, my lunch consisted of a salad with avocado, a veggie (either mushrooms or bell peppers) and more sausage, snacks were usually string cheese or something equally low carb, and dinner was a meat and a veggie. My main source of carbohydrates was the air-popped popcorn I eat nearly every night. It’s my one vice, leave me alone.
Here is a snapshot of those 5 days (Monday, August 8-August 12).

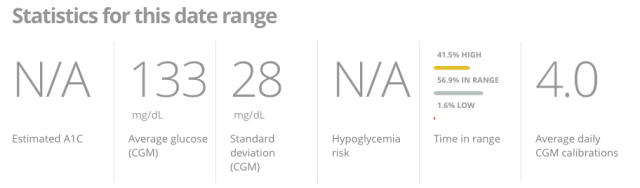
An average glucose of 133 mg/dl equals an A1C of 6.3%. One of my CDEs, Jenny Smith at Integrated Diabetes Service, says that I should aim for a standard deviation of less than 25. Not too shabby at 28. And I spent 56% of the time in range, and although it says 41.5% of my blood sugars are high, it turns out that 37.9% of those blood sugars are between 140-180 and only 4.5% of my highs are above 180 mg/dl.
Now, on Sunday I had another big brunch here at the house, and then my husband went out of town on a business trip. We had a lot of leftovers, so I though I could swing it by just eating what we had. It mostly involved lots of toast for breakfast, crackers and more toast during the day (I went to Chipotle for a salad once), and then macaroni and cheese and leftover birthday cupcakes in the evening. As you can imagine, it didn’t go so well. Even with my attempts at temp basaling and bolusing the shit out of this food, I didn’t do so well.
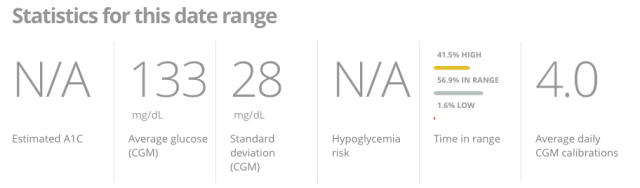
Here is a snapshot of Monday, August 14-Thursday, August 18:


An average blood sugar of 151 mg/dl is equal to 6.9%, and while yes, my A1C is still predicted to be in the 6s, my standard deviation is now double what it should be. In addition, I’m now spending only 41.2% of the time in range, time low jumped from 1.6% to 4.4%, and I’m high more than half the time at 54.5%. My time between 140 and 180 dropped 10% to 27.3% and my time over 180 jumped from 4.5% to a whopping 27.9%.
You guys, my time spent over 180 mg/dl this week didn’t just double, it increased by 6x!
Okay, so one caveat I want to make is that I stayed high throughout the night because for two nights, I forgot to turn off the vibrate-only setting on my Dexcom, so I never had a chance to correct so it potentially could have been lower. But if you look at least weeks, my blood sugars never went so high overnight that I would have needed to correct. Week 1 is clearly superior to Week 2. You can also see that my highs during the day were much higher and last much longer than the highs from Week #1.
So what does this tell me? Well, it tells me that I need to eat low-carb. Yes, I understand that on very special occasions, like my birthday, I can treat myself. But I can’t pretend it’s my birthday for an entire week (or month…) even though it’s really fun. Recovering from one blood sugar indiscretion is a lot easier than recovering from five days in a row.
One of the biggest lessons I learned from comparing this week and last week isn’t just how my blood sugar responds to different foods, it’s realizing how much time I spend worrying about my blood sugars and how frustrated I get with this disease when I try to act like I don’t have it. It really sucks to admit it, but I do have diabetes and it does actually require me to live my life a little differently than everyone else.
But you know what? So what. Most people can’t do whatever they want because of how their choices will affect them and others. Whether it’s gaining weight or having some kind of food allergy, there are so many people who have to say, “No, I’m sorry, I can’t eat that.” And yes, okay, maybe I can eat that. But do I want to? Do I really want to eat that and then deal with the consequences? We use that term bolus-worthy and I used to think it was cute but I’m not sure I really ever understood it’s definition. What I think it should be is “Is it work-worthy?” because what it takes to have “normal blood sugars” while “eating normally” is that it usually takes a lot of time and effort, with a high risk and usually very little reward.
Am I solidly in the low carb club? Hardly. I don’t think you’re going to hell if you don’t have an A1C in the 5s and I’m not going to try to cast demons out of you if you eat a sandwich. But I do think my priorities are changing. Right now my focus is getting an A1C in the 6s so that I can successfully carry a healthy baby to term. But I am also realizing what a relief on the mental burden of diabetes it is to eat low carb. Because I’m not fighting against my body’s natural inclination to have high blood sugar. The stress and frustration of trying to accurately guesstimate carbs is virtually eliminated. The unknowns of “when is this going to kick in?” or “What kind of temp basal should I use?” or “Am I going to crash at 4 am?” are gone. Everything feels a little more, well, manageable.
I really wanted to believe that people with diabetes could eat anything they wanted, any time they wanted. But I don’t think that’s true and I think most of us know it’s not true. I know a lot of people who have said there are certain things they’ve given up eating because it’s too hard. And I think that’s really what it comes down to. The work. The stress. The success rate. Is it worth the work?
I would never tell anyone to do or not to do something, because that’s not my place. But I would encourage a bit of self-reflection on what’s working. What’s actually working, not what you’ve been told by, well, anyone. You are n=1. You are the only one you need to worry about when it comes to what you can or can’t, should or shouldn’t, will or won’t do. Don’t listen to me, don’t listen to your Facebook groups, don’t listen to your doctor (well, except for the whole taking your insulin thing, please keep doing that). If someone says “You should do this” and it’s not working, it’s not your fault. You didn’t do something wrong, you didn’t fail at life. It’s just you and how you work and what you need to be healthy and reach your goals. And that’s the only end result you should be looking at.













 It’s no secret that I have been writing about diabetes, in one way or another, for a long time. About half my life, actually. And I’ve had the disease itself for about three-quarters of my life. That’s a lot of time centered around one not-so-great aspect of my otherwise very full and happy existence.
It’s no secret that I have been writing about diabetes, in one way or another, for a long time. About half my life, actually. And I’ve had the disease itself for about three-quarters of my life. That’s a lot of time centered around one not-so-great aspect of my otherwise very full and happy existence.